As per the American Heart Association (AHA), if you are an adult, your heart rate should be in the range of 60 to 100 beats per minute. And if your age is between 6 and 15 years, your heart rate should be anywhere between 70 and 100 per minute. What is a good heart rate for my age? The audibility of heartbeat mostly depends on the fetal position and nature of abdominal tissues. Also, a normal heartbeat lowers the risk of miscarriage. Baby’s Heart Beat At Birth. The newly born’s (neonate) heart rate while awake is 100 to 165bpm and while sleeping is 90 to 160bpm. This is during the first 28 days of a baby’s life.

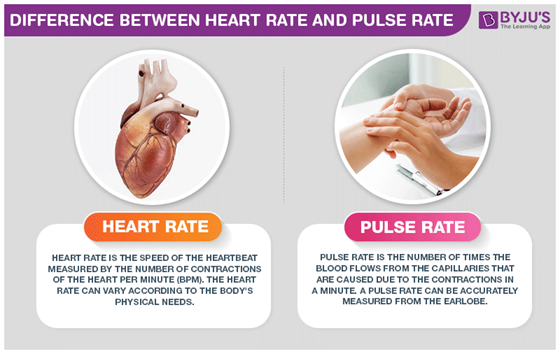
A normal resting heart rate for adults ranges from 60 to 100 beats per minute. Generally, a lower heart rate at rest implies more efficient heart function and better cardiovascular fitness. For example, a well-trained athlete might have a normal resting heart rate closer to 40 beats per minute. To measure your heart rate, simply check your pulse. Your pulse rate is the number of times your heart beats per minute. A normal resting heart rate should be 60–100 beats per minute, but it can vary from minute to minute. It can go up to 130–150 beats or higher per minute when you’re exercising – that’s normal because the body needs to pump more oxygen-rich blood around the body. The typical range of 60 to 100 beats per minute is both the average pulse measurement as well as the rate at which most people’s heart needs to beat to pump enough blood through their body.
By Julia H. Indik, MD, PhD, associate professor of medicine, University of Arizona Sarver Heart Center
The normal heart beat begins in the sinus node, located near the top of the right atrium. (See Figure below.) This electrical impulse spreads over the atrium, causing the atria to contract to pump the blood into the ventricles. But for the atrial impulse to get to the ventricles, it must go through the AV node and the His Bundle. The electrical impulse then travels down the bundle branches to the ventricular muscles, causing them to contract, producing a heartbeat that pumps the blood to the body. The normal heart rate is between 60 and 100 beats per minute.
If the sinus node is without nerves (for example a transplanted heart) the heart rate is about 80 beats per minute. Two types of nerves regulate the heart rate. The sympathetic nerve speeds up the heart rate with exertion or excitement. The vagal nerves slow the heart rate. Many athletes have a slow heart rate due to increased vagal tone. In non-athletes a slow heart rate can be a sign of a defective AV node. The heart rate also can be increased by adrenalin from the adrenal glands, due to exercise or excitement.
Normal conduction from the atrium to the ventricles
The electrical heart. Each heart beat is started electrically at the sinus node. Then the electrical impulse is carried to the AV node and relayed to the ventricles over the left and right bundle branches to the heart muscle.
Slow Heart Beat (Bradycardia)
An abnormally slow sinus heart rate is called the “sick sinus syndrome” and, if severe, results in symptoms of fatigue. In some such cases a permanent pacemaker is needed to be implanted to generate a normal heart rate. Many people with sick sinus syndrome also develop atrial fibrillation. These individuals have intermittent heart rates that are often either too fast or too slow.
Normal Heart Rate By Age
From the atrium, the electrical impulse is carried through the AV node, which sits as an electrical “relay” between the upper chambers (atria) and lower chambers (ventricles). Slowdown in the AV node can be another cause for bradycardia, in which not all the sinus node discharges can make it through to the ventricle, a form of heart block. Sometimes the AV node slows down due to medications, which need to be adjusted.
After the AV node, comes the left and right bundle branches, very important electrical relays that are the final pathways to signal the ventricles to beat. A slowdown or block in this part of the conduction system may be serious and require a pacemaker as some patients can develop “complete heart block.” In complete heart block, no signals from the sinus node can penetrate to the ventricles, and the patient can have a dangerously slow pulse. Adjusting medications cannot fix this type of complete heart block; a pacemaker is needed.
Treating Slow Heart Rhythms
Sometimes a slow heart beat can be improved by adjusting medications. This may be the case with “sick sinus syndrome,” for example. When the slow heart beat cannot be improved by medication adjustments, a pacemaker is needed. Pacemakers also are needed when signals from the atrium are not conducted to the atrium; this is known as “complete heart block.”
Placing a pacemaker: Pacing leads (one to three) are positioned through the vein under the collarbone (subclavian vein) into the heart chambers and affixed to the heart muscle. These leads then are connected to the pacemaker generator, which is placed under the skin in the front chest region just below the collarbone. This procedure is performed in the electrophysiology laboratory and typically takes about one to two hours. If a third lead is needed for what is called “biventricular pacing” for heart failure, the procedure may take up to three hours.
Follow up and monitoring: The patient will have future follow-up appointments in the pacemaker clinic and can be followed remotely with a home monitoring unit. Very little in the typical environment interferes with a pacemaker. It is fine to use microwaves and cell phones, but not placing the cell phone directly over the device. A patient with a pacemaker cannot get an MRI, but a CT scan is all right. At the airport, the device will set off the metal detectors, so inform security that you have a pacemaker. At stores with anti-theft devices at the door, patients should simply walk through and not linger by the door.
Fast Heart Rhythms – Tachycardia
Tachycardia refers to a situation where the pulse is faster than 100 beats per minute (bpm). Sometimes this is absolutely normal. For instance, with exercise it is entirely appropriate for the pulse to rise above 100 bpm. However, when tachycardia occurs at rest, a cardiologist needs to determine the specific cause.
The first question is whether the tachycardia is originating from the upper chambers (“atria”) or the lower chambers (“ventricles”). Ventricular tachycardia refers to a fast heart beat that originates from the ventricles and can be potentially dangerous.

If tachycardia originates from the upper chambers, it will be one of three types:
1) Atrial fibrillation
2) Atrial flutter
3) Supraventricular tachycardia (SVT for short)
Atrial fibrillation is a chaotic, electrical disturbance of the atria in which an electrical impulse travels in a disorganized, very rapid fashion throughout the atrium. This electrical impulse then travels to the AV node and the rest of the conduction system to the lower chambers (ventricles) in an irregular fashion, resulting in a heartbeat that is perceived as irregular and often fast. It is the most common rhythm disturbance in older Americans, affecting 2.2 million Americans with an average age of about 75 years. Some people are very aware of their atrial fibrillation – they notice that their heart is beating very irregularly, without any pattern whatsoever and fast. Other people are completely unaware of being in atrial fibrillation. Most people are aware of this rhythm some of the time, but not at other times, even when they are certain that they can detect it “perfectly.”
Atrial fibrillation puts people at significant risk for a stroke. So, medical guidelines advise medication to thin the blood for those at risk for stroke. Some patients can be treated with aspirin, depending on their doctor’s assessment.
Atrial flutter is a heart rhythm disturbance that is similar to atrial fibrillation, except that the electrical discharges are semi-organized. An electrical impulse will typically revolve around the tricuspid valve. Patients with atrial flutter may feel the same symptoms as those with atrial fibrillation – a fast and irregular heartbeat, though maybe not quite as irregular. Atrial flutter also carries a potential risk for stroke and all the same indications for blood thinners, as outlined above, still apply.
Supraventricular tachycardia (SVT) is a fast heart rhythm disturbance that can be seen at any age. People will describe that their heart suddenly starts racing –it goes from a normal 60 beats per minute to as much as 150 to 200 beats per minute, and then stops just as abruptly.
Ventricular Tachycardia, which originates from the ventricles and is related to the lethal rhythm called ventricular fibrillation is the most critical and potentially dangerous of the lower-chamber tachycardias. Cardiac arrest in this country often is caused by these types of serious rhythm disturbances, so making an accurate diagnosis is very important. Ventricular tachycardia usually occurs in people who are having or who have had heart attacks.
Treating Fast Heart Rhythms
Many patients with a risk for ventricular tachycardia or ventricular fibrillation also have heart failure and may benefit from a device called an implantable cardiac defibrillator (ICD). An ICD is similar to a pacemaker, but larger. It monitors the heart rhythm to detect ventricular fibrillation or ventricular tachycardia and delivers therapy—rapid pacing or a shock—to restore a normal rhythm. The device is implanted in the upper chest below the collarbone, as is a pacemaker.
Biventricular pacing or “cardiac resynchronization therapy” is a special type of device that is usually coupled with an ICD to treat heart failure patients who have severe symptoms related to their heart failure and have evidence of an electrical condition called “left bundle branch block.” In this type of block, the electrical signal travels very slowly from the right side to the left side of the heart, causing the heart muscle to contract in an uncoordinated fashion. A pacing lead can be placed from a vein inside the heart to the left side of the heart to re-coordinate the heart and to improve symptoms of shortness of breath.
Electrophysiology (EP) Study and Ablation. This is a procedure where a fast heart rhythm problem can be treated by directly burning (cauterizing), or heating, the muscle tissue that is responsible for the problem. Cardiologists use x-rays to guide placement of catheters (small “spaghetti-sized” electrodes) into the veins (and sometimes artery) in the upper thighs of the legs. The catheters are positioned inside the heart in specific locations to record the electrical signals. Doctors then induce tachycardia and analyze how the heart is electrically activated to determine the areas that are responsible for starting or perpetuating the abnormal rhythm. Energy (typically radiofrequency) is then applied at that spot to cauterize the muscle tissue responsible for the abnormal rhythm. The success rate depends on the type of heart rhythm problem being treated and is greater than 90 percent for most heart rhythm problems. For ablation of atrial fibrillation, the success rate depends on the nature of the problem, but is usually between 60 and 80 percent.
By Julia H. Indik, MD, PhD, associate professor of medicine, University of Arizona Sarver Heart Center
The normal heart beat begins in the sinus node, located near the top of the right atrium. (See Figure below.) This electrical impulse spreads over the atrium, causing the atria to contract to pump the blood into the ventricles. But for the atrial impulse to get to the ventricles, it must go through the AV node and the His Bundle. The electrical impulse then travels down the bundle branches to the ventricular muscles, causing them to contract, producing a heartbeat that pumps the blood to the body. The normal heart rate is between 60 and 100 beats per minute.
If the sinus node is without nerves (for example a transplanted heart) the heart rate is about 80 beats per minute. Two types of nerves regulate the heart rate. The sympathetic nerve speeds up the heart rate with exertion or excitement. The vagal nerves slow the heart rate. Many athletes have a slow heart rate due to increased vagal tone. In non-athletes a slow heart rate can be a sign of a defective AV node. The heart rate also can be increased by adrenalin from the adrenal glands, due to exercise or excitement.
Normal conduction from the atrium to the ventricles
The electrical heart. Each heart beat is started electrically at the sinus node. Then the electrical impulse is carried to the AV node and relayed to the ventricles over the left and right bundle branches to the heart muscle.
Slow Heart Beat (Bradycardia)
An abnormally slow sinus heart rate is called the “sick sinus syndrome” and, if severe, results in symptoms of fatigue. In some such cases a permanent pacemaker is needed to be implanted to generate a normal heart rate. Many people with sick sinus syndrome also develop atrial fibrillation. These individuals have intermittent heart rates that are often either too fast or too slow.
From the atrium, the electrical impulse is carried through the AV node, which sits as an electrical “relay” between the upper chambers (atria) and lower chambers (ventricles). Slowdown in the AV node can be another cause for bradycardia, in which not all the sinus node discharges can make it through to the ventricle, a form of heart block. Sometimes the AV node slows down due to medications, which need to be adjusted.
After the AV node, comes the left and right bundle branches, very important electrical relays that are the final pathways to signal the ventricles to beat. A slowdown or block in this part of the conduction system may be serious and require a pacemaker as some patients can develop “complete heart block.” In complete heart block, no signals from the sinus node can penetrate to the ventricles, and the patient can have a dangerously slow pulse. Adjusting medications cannot fix this type of complete heart block; a pacemaker is needed.
Treating Slow Heart Rhythms
Sometimes a slow heart beat can be improved by adjusting medications. This may be the case with “sick sinus syndrome,” for example. When the slow heart beat cannot be improved by medication adjustments, a pacemaker is needed. Pacemakers also are needed when signals from the atrium are not conducted to the atrium; this is known as “complete heart block.”
Placing a pacemaker: Pacing leads (one to three) are positioned through the vein under the collarbone (subclavian vein) into the heart chambers and affixed to the heart muscle. These leads then are connected to the pacemaker generator, which is placed under the skin in the front chest region just below the collarbone. This procedure is performed in the electrophysiology laboratory and typically takes about one to two hours. If a third lead is needed for what is called “biventricular pacing” for heart failure, the procedure may take up to three hours.
Follow up and monitoring: The patient will have future follow-up appointments in the pacemaker clinic and can be followed remotely with a home monitoring unit. Very little in the typical environment interferes with a pacemaker. It is fine to use microwaves and cell phones, but not placing the cell phone directly over the device. A patient with a pacemaker cannot get an MRI, but a CT scan is all right. At the airport, the device will set off the metal detectors, so inform security that you have a pacemaker. At stores with anti-theft devices at the door, patients should simply walk through and not linger by the door.
Fast Heart Rhythms – Tachycardia
Tachycardia refers to a situation where the pulse is faster than 100 beats per minute (bpm). Sometimes this is absolutely normal. For instance, with exercise it is entirely appropriate for the pulse to rise above 100 bpm. However, when tachycardia occurs at rest, a cardiologist needs to determine the specific cause.
The first question is whether the tachycardia is originating from the upper chambers (“atria”) or the lower chambers (“ventricles”). Ventricular tachycardia refers to a fast heart beat that originates from the ventricles and can be potentially dangerous.
If tachycardia originates from the upper chambers, it will be one of three types:
1) Atrial fibrillation
2) Atrial flutter
3) Supraventricular tachycardia (SVT for short)
Atrial fibrillation is a chaotic, electrical disturbance of the atria in which an electrical impulse travels in a disorganized, very rapid fashion throughout the atrium. This electrical impulse then travels to the AV node and the rest of the conduction system to the lower chambers (ventricles) in an irregular fashion, resulting in a heartbeat that is perceived as irregular and often fast. It is the most common rhythm disturbance in older Americans, affecting 2.2 million Americans with an average age of about 75 years. Some people are very aware of their atrial fibrillation – they notice that their heart is beating very irregularly, without any pattern whatsoever and fast. Other people are completely unaware of being in atrial fibrillation. Most people are aware of this rhythm some of the time, but not at other times, even when they are certain that they can detect it “perfectly.”
Atrial fibrillation puts people at significant risk for a stroke. So, medical guidelines advise medication to thin the blood for those at risk for stroke. Some patients can be treated with aspirin, depending on their doctor’s assessment.
Atrial flutter is a heart rhythm disturbance that is similar to atrial fibrillation, except that the electrical discharges are semi-organized. An electrical impulse will typically revolve around the tricuspid valve. Patients with atrial flutter may feel the same symptoms as those with atrial fibrillation – a fast and irregular heartbeat, though maybe not quite as irregular. Atrial flutter also carries a potential risk for stroke and all the same indications for blood thinners, as outlined above, still apply.
Normal Values For Heart Rate
Supraventricular tachycardia (SVT) is a fast heart rhythm disturbance that can be seen at any age. People will describe that their heart suddenly starts racing –it goes from a normal 60 beats per minute to as much as 150 to 200 beats per minute, and then stops just as abruptly.
Ventricular Tachycardia, which originates from the ventricles and is related to the lethal rhythm called ventricular fibrillation is the most critical and potentially dangerous of the lower-chamber tachycardias. Cardiac arrest in this country often is caused by these types of serious rhythm disturbances, so making an accurate diagnosis is very important. Ventricular tachycardia usually occurs in people who are having or who have had heart attacks.

Treating Fast Heart Rhythms
Many patients with a risk for ventricular tachycardia or ventricular fibrillation also have heart failure and may benefit from a device called an implantable cardiac defibrillator (ICD). An ICD is similar to a pacemaker, but larger. It monitors the heart rhythm to detect ventricular fibrillation or ventricular tachycardia and delivers therapy—rapid pacing or a shock—to restore a normal rhythm. The device is implanted in the upper chest below the collarbone, as is a pacemaker.
Biventricular pacing or “cardiac resynchronization therapy” is a special type of device that is usually coupled with an ICD to treat heart failure patients who have severe symptoms related to their heart failure and have evidence of an electrical condition called “left bundle branch block.” In this type of block, the electrical signal travels very slowly from the right side to the left side of the heart, causing the heart muscle to contract in an uncoordinated fashion. A pacing lead can be placed from a vein inside the heart to the left side of the heart to re-coordinate the heart and to improve symptoms of shortness of breath.
Normal Heart Beat Per Minute For Fetus
Electrophysiology (EP) Study and Ablation. This is a procedure where a fast heart rhythm problem can be treated by directly burning (cauterizing), or heating, the muscle tissue that is responsible for the problem. Cardiologists use x-rays to guide placement of catheters (small “spaghetti-sized” electrodes) into the veins (and sometimes artery) in the upper thighs of the legs. The catheters are positioned inside the heart in specific locations to record the electrical signals. Doctors then induce tachycardia and analyze how the heart is electrically activated to determine the areas that are responsible for starting or perpetuating the abnormal rhythm. Energy (typically radiofrequency) is then applied at that spot to cauterize the muscle tissue responsible for the abnormal rhythm. The success rate depends on the type of heart rhythm problem being treated and is greater than 90 percent for most heart rhythm problems. For ablation of atrial fibrillation, the success rate depends on the nature of the problem, but is usually between 60 and 80 percent.
